How Has Medicaid Changed Over The Years For Long Term Care
Every bit states face their nearly challenging budgets in decades alongside new responsibilities to implement national wellness reform, many are looking at opportunities to improve long-term care equally a way to control costs and serve seniors and people with disabilities in the settings they adopt. This issue of States in Action describes provisions in the Affordable Care Human activity that assistance states in expanding home- and community-based long-term intendance services, the growing grassroots movement to improve facility-based intendance, and innovative programs in Colorado, Michigan, and Rhode Island that seek to provide consumer-directed long-term care.
Long-Term Care Services and Supports
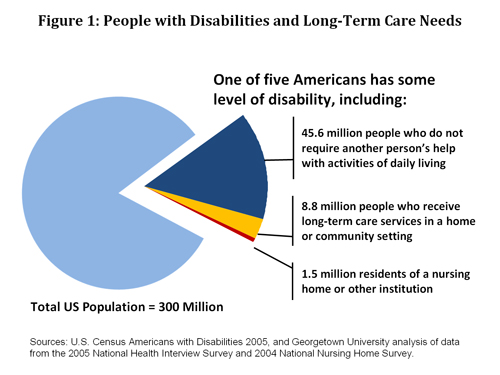
One of 5 Americans—56 million people—written report having a inability that limits routine activities of daily living. Among this population, about 10.three million people crave long-term intendance, which includes a variety of medical and social services to help come across health or personal needs. About long-term intendance is to assist people with basic tasks, such as eating or bathing, or activities necessary for independence, such as preparing meals or managing coin. And well-nigh people who demand long-term intendance services and supports (85%) receive them at home or in community-based settings, such as a daytime activity eye. However, a significant number of people who require long-term care—1.5 million—reside in nursing homes or other facilities that attend to their long-term care needs (Effigy i).
Most long-term intendance is provided as unpaid help from family and friends: four of v people who receive long-term care in the community rely exclusively on unpaid help (National Clearinghouse for LTC). When unpaid assistance is non enough or not available, then people with disabilities rely on paid individuals or companies to provide services. These services are expensive and can quickly exhaust lifetime savings. When that happens, the Medicaid and Medicare programs provide assistance.
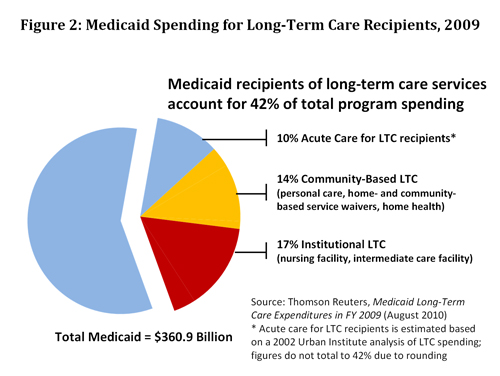
Medicaid pays the greatest share of total U.S. long-term care spending (forty%), almost double the share paid past Medicare (23%) or individuals and families (22%) and more than than three times that paid by private insurance (12%) (KCMU). In 2009, Medicaid spent $114.1 billion on long-term care services and supports, including $fifty billion for customs-based services and $63 billion for facility-based services. In addition, Medicaid spent approximately $38 billion on acute-care services for recipients of long-term care. Overall, Medicaid beneficiaries who receive long-term intendance services accounted for 42 percent of total Medicaid spending in 2009 (Figure 2).
Expanding Dwelling house- and Community-Based Services
Over the by three decades, states accept been expanding Medicaid home- and community-based services (HCBS) in response to consumer preferences for alternatives to facility-based long-term care and, since 1999, in response to court-ordered mandates to serve people with disabilities in the least restrictive setting, taking into business relationship the resource of the state. State Medicaid spending on HCBS programs has increased dramatically over the past ten years, from 27 per centum of full long-term care spending in 1999 to 44 percent in 2009 (Thomson Reuters). The shift toward HCBS as well represents a budget strategy in most states to decrease Medicaid spending on higher-cost, facility-based services.
National health reform creates a number of opportunities for states to further expand access to HCBS programs. "I know, equally a one-time governor," said Health and Human being Services Secretarial assistant Kathleen Sebelius in a July 26 letter to governors, "that the federal authorities and states need to work adjacent to deliver on the Affordable Intendance Act's promise of access to wellness intendance regardless of inability" and "provide greater opportunities for Americans with disabilities to live and piece of work in their communities." The ACA creates new HCBS benefit options, higher income eligibility standards for these services, and federal financial incentives for states to further shift or "rebalance" long-term care budgets toward community-based settings. Major HCBS initiatives in the new police force include:
- HCBS State Plan Selection. Department 2402 (folio 211) provides states with new flexibility to expand HCBS benefits and fiscal eligibility through a Medicaid state program amendment instead of the more restrictive waiver procedure. However, this option includes new restrictions some states may detect troubling. If a state creates an HCBS program using this option, information technology will automatically create an "entitlement" to that program and (unlike waiver programs) volition be required to operate the program uniformly statewide without waiting lists. (At that place is more information nearly this option here.)
- Community First Pick Option. Section 2401 (folio 206) allows states to provide HCBS bellboy supports and services through a land plan amendment and receive a six percentage signal increase in the Federal Medicaid Assist Percentages (federal matching funds) for those services. This option also results in an entitlement that requires attendant services under the state plan to be offered uniformly statewide without waiting lists.
- Money Follows the Person Demonstration. Section 2403 (page 214) extends to 2016 the Coin Follows the Person (MFP) rebalancing demonstration created through the Deficit Reduction Human activity of 2005. MFP provides states with enhanced federal matching funds for 12 months for each Medicaid casher transitioned from an institution to the community during the demonstration period. (There is more information nearly this option here.)
- State Balancing Incentive Program. Section 10202 (page 845) provides enhanced federal matching payments to states to increase the proportion of Medicaid long-term intendance dollars that go toward HCBS. States that currently spend less than fifty percent of their Medicaid long-term intendance upkeep on HCBS are eligible to receive a two percentage betoken increase in federal matching funds on all HCBS programs, including waivers, mandatory domicile health benefits, optional personal care benefits, cocky-directed personal assistance services, and Programs of All-Inclusive Care for the Elderly (Step). Eligibility for the enhanced match has not been determined, merely will probable reflect HCBS spending reported hither.
Changing the Culture of Residential Care
"States need to be careful not to focus too narrowly on just HCBS options," says Bonnie Kantor, executive manager of the Pioneer Network. "Instead of focusing on the setting of care," she says, "the existent goal is to create a culture of patient-centered intendance that creates a sense of domicile and community in every setting, including facility-based care."
This is particularly important for older adults, who are more likely than younger adults to receive facility-based long-term intendance: 22 percent of people age 65 and older who demand long-term care reside in a facility, compared with only 4 percent of those under age 65, co-ordinate to a Georgetown University analysis. Older adults' greater reliance on facility-based long-term intendance besides is evident in Medicaid spending. Facility-based intendance accounts for 66 percentage of Medicaid long-term intendance spending for older adults and people with physical disabilities, compared with 34 pct for people with intellectual and other developmental disabilities, who every bit a group are younger.
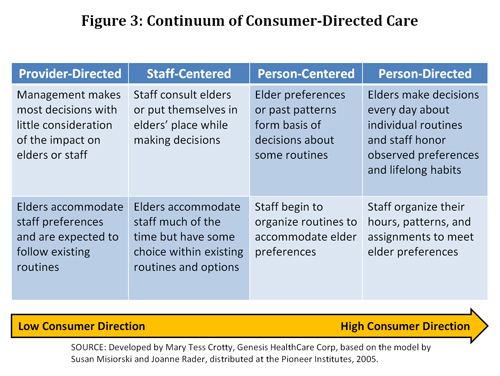
Consumers, patient advocates, providers, and policymakers are calling for "civilization alter" to improve long-term care. (See Ask the Proficient for further description of the civilisation alter motion.) The Pioneer Network, which focuses on culture change for seniors, was an early advocate of moving from provider-directed intendance toward consumer-directed care that preserves the dignity of individuals and enables them to make decisions most their daily routines (Figure three). The provisions of the national wellness reform police force described in a higher place promote culture modify by seeking to integrate care around the person, increase workforce capacity, and improve the quality of care.
Civilization change has begun to receive meaning attending at the national and state levels. Philanthropic foundations, including The Commonwealth Fund, are funding programs to help foster culture change in nursing homes and other long-term care settings. At the federal level, the Centers for Medicare and Medicaid Services (CMS) has contracted with quality comeback organizations to train providers to appoint in culture change efforts and sponsored several national meetings to bring the major stakeholders together. The Found for Aging Services reports on these activities hither.
Given that states are major players in financing and regulating long-term care, they take an of import role to play in ensuring the quality of care and quality of life that people receive in nursing homes and other long-term intendance settings. Opportunities for states to improve long-term care services and support systems are described in the Ask the Expert column and Snapshots in this upshot.
Source: https://www.commonwealthfund.org/publications/newsletter-article/national-health-reform-and-long-term-care
Posted by: thompsonmecer1954.blogspot.com


0 Response to "How Has Medicaid Changed Over The Years For Long Term Care"
Post a Comment